Some people believe that health is purely biological, assuming that thoughts and feelings are separate from the body.
French philosopher René Descartes popularised this dualistic (and false) notion back in 1641, and Western medicine has essentially followed this path ever since. While Eastern traditions have consistently recognised the unity of mind and body, Western medicine has only recently started to incorporate this vital understanding; however, there is still a long way to go.
Connecting the two is known as holistic, which comes from the Greek word holos, meaning whole, thus dealing with the person as a unified whole. Hypnotherapy is a holistic therapy.
When the Mind Affects the Body
Two pathways describe how psychological factors influence physical symptoms:
- Psychogenic – symptoms originate in the mind but appear in the body. Example: persistent back pain without detectable injury.
- Psychosomatic – illness is physical but worsened or triggered by mental states. Example: ulcers caused by the H. pylori bacteria are often aggravated by stress.
The subconscious controls many of these effects, shaping thought patterns, bodily reactions, and the healing process. Research in Psychoneuroimmunology (PNI) indicates that unresolved stress disrupts hormone balance, suppresses immunity, and promotes inflammation – changes that increase disease risk over time.
Stress and Hormones
Chronic stress elevates cortisol and adrenaline, which in turn raise blood pressure and strain the heart. The Interheart study (Rosengren et al., Lancet, 2004) linked psychosocial stress to an increased global risk of heart attacks. Stress also disrupts the HPA axis, weakening immunity. A meta-analysis (Segerstrom & Miller, Psychol Bull, 2004) confirmed that long-term stress makes people more susceptible to illness.
Early-Life Trauma
The Adverse Childhood Experiences (ACE) Study (Felitti et al., Am J Prev Med, 1998) showed that childhood abuse, neglect, or hardship increases adult risk of heart disease, diabetes, and cancer. Trauma can recalibrate the stress response system and even alter gene expression through epigenetic mechanisms.
Trauma, PTSD, and Inflammation
In PTSD, the body stays locked in fight, flight or freeze mode, creating chronic inflammation. Studies link PTSD to autoimmune disease, cardiovascular problems, and chronic fatigue (Lindqvist et al., Biol Psychiatry, 2017).
Stress, Anxiety, and the Gut
Stress alters the gut–brain axis, affecting microbes and sensitivity, and worsening IBS and IBD. Mayer (Gastroenterology, 2011) described stress as a key factor in IBS. Anxiety also contributes to reflux and ulcer flare-ups.
Depression and Immunity
Depression dampens immune defences by reducing natural killer (NK) cell activity. This weakens resistance to infections and cancer. Antoni et al. (Nat Rev Cancer, 2006) found that stress and depression can accelerate disease progression.
Loneliness and Burnout
Loneliness is now recognised as a mortality risk. Holt-Lunstad et al. (PLoS Med, 2010) reported that isolation increases early death, partly through stress-related immune decline. Burnout, marked by exhaustion, also impairs mitochondrial energy production, contributing to chronic fatigue–like symptoms (Bianchi et al., Neurosci Biobehav Rev, 2017).
Trauma and the Body’s Surface
Psychological stress can trigger physical flare-ups such as non-epileptic seizures or skin conditions like eczema and psoriasis. These reflect nervous–immune–skin interactions (Arck et al., J Invest Dermatol, 2006).
Conclusion:
Research across various medical fields points to the same conclusion: emotional distress does not stay confined to the mind—it affects the body. Stress and trauma influence hormones, immunity, and inflammation, increasing the risk of heart disease, autoimmune conditions, digestive issues, cancer progression, chronic pain, and skin problems. Effective healing requires addressing both emotional and physical aspects.
When medicine cannot explain symptoms, exploring a person’s beliefs, early experiences, and emotional history often uncovers the missing link, where mind-body therapy (like hypnotherapy) and medical care need to connect.

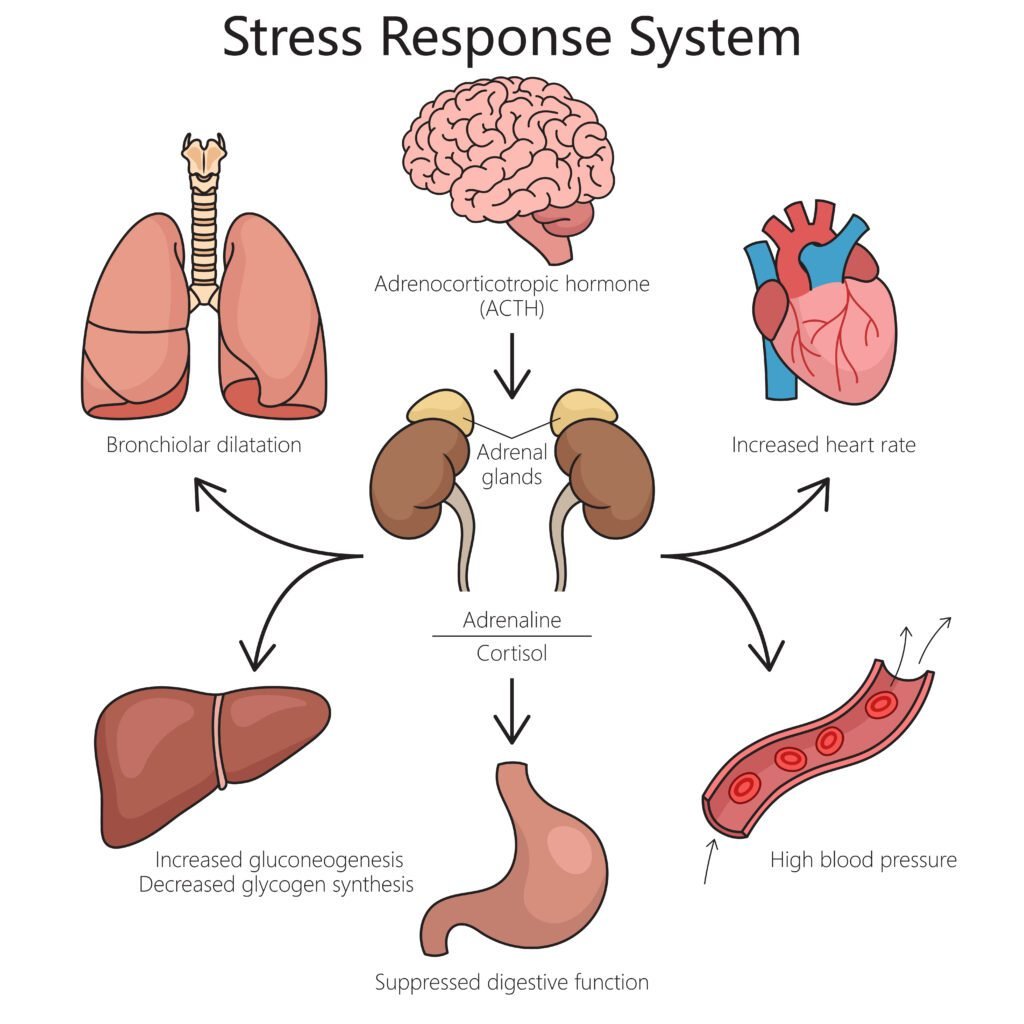
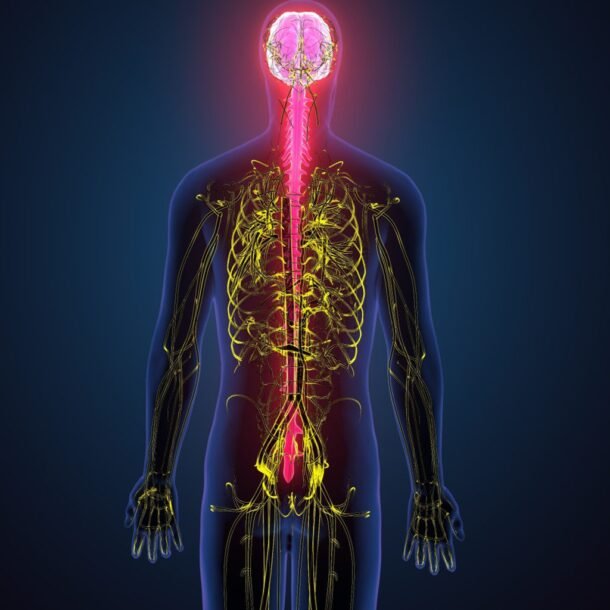
In the brain, the Diencephalon functions like a telephone switchboard, connecting the body’s signals to the subconscious mind, mainly to the hypothalamus and thalamus. It also communicates with the limbic system and brainstem in a two-way flow of information and activation (of mRNA to peptides, etc.).
Thus, the mind, nerve, hormone, immune, and blood systems function in (homeostatic) balance with one another for our overall wellbeing. However, unresolved, unhelpful beliefs and highly emotional, traumatic memories (in the limbic system) can dysregulate this system (e.g. persistent stress increases cortisol release, a hormone that suppresses the immune system and disrupts metabolism), leading to declining physical health or coping abilities (self-management, relationships, etc.) over time, when therapy is advisable to deal with it (in various ways); with medical care, where necessary.
Kail Shanker, Oct. 2025
